Prediction and Prevention of Non-Adherence to Digital Health Interventions
Digital health interventions (DHIs) show vast potential in supporting patients and health care systems with the globally increasing prevalence and economic costs of non-communicable diseases (NCDs) – the leading causes of death and disability worldwide [1, 2]. More specifically, Mobile Health Applications (mHealth apps) are now considered an accessible and scalable solution to promote behavior change among patients, improve health outcomes, and reduce healthcare costs [3-5]. Correspondingly, the number of available mHealth apps has continuously grown to more than 300.000, with approximately 200 new mHealth apps released each day [2, 6].
However, despite increasing evidence and availability, mHealth apps are subject to significant dropout rates, with a substantial proportion of users not adhering to them as intended [7, 8]. Recent research has shown that up to 80 percent of all participants in mHealth interventions only engage at a minimum level, not logging into the mHealth app more than once and not consistently using the app long term [9]. Studies examining mHealth app usage in more extensive real-world settings further show that less than five percent of participants are daily active users, with the large majority only downloading the corresponding app but not using it regularly [10, 11].
Since non-adherence relative to intended use jeopardizes treatment success and thus might lead to an increased number of hospitalizations, it is considered a fundamental concern in developing mHealth apps [8, 12-15]. Still, the scientific body of literature lacks concise conceptualizations and measures for intended use of mHealth apps, while intervention components and other factors influencing adherence remain to be explored [13, 16].
Therefore, understanding factors that act as barriers or facilitators to adherence is crucial to prevent intervention dropouts and increase the effectiveness of digital health interventions. Furthermore, identifying users at risk and preventing them from dropping out indicates the potential to increase the efficiency and quality of DHIs as many interventions are only beneficial if people use them regularly and for a prolonged period [14, 15, 17-19].
Research Objectives
Predicting and preventing intervention dropouts and thus increasing the effectiveness of mHealth apps requires multiple steps: First, understanding the factors that act as barriers or facilitators to user adherence. Second, being able to predict dropouts based on individual real-time data. Third, incorporating effective preventive intervention components and actions that induce behavior change at the right time before the dropout occurs. To this end, we will use our technical expertise in the state of receptivity to fill this research gap and apply it to the prediction and prevention of non-adherence [20, 21].
In this regard, our project has the following objectives:
- Identifying factors that influence adherence and predict dropouts based on existing literature and real-world data from longitudinal studies of different health domains.
- Identifying intervention components that effectively intervene in critical situations to prevent dropout
- Developing and evaluating an early warning system that can predict and prevent dropouts.
From a practical perspective, these objectives aim to help stakeholders of DHIs in developing more compelling and effective mHealth apps.
Planned Studies and Research Questions
We are planning three distinct studies which combine evidence from the existing body of research, retrospective analysis of longitudinal data from real-world mHealth apps, and prospective data analysis to validate our findings.
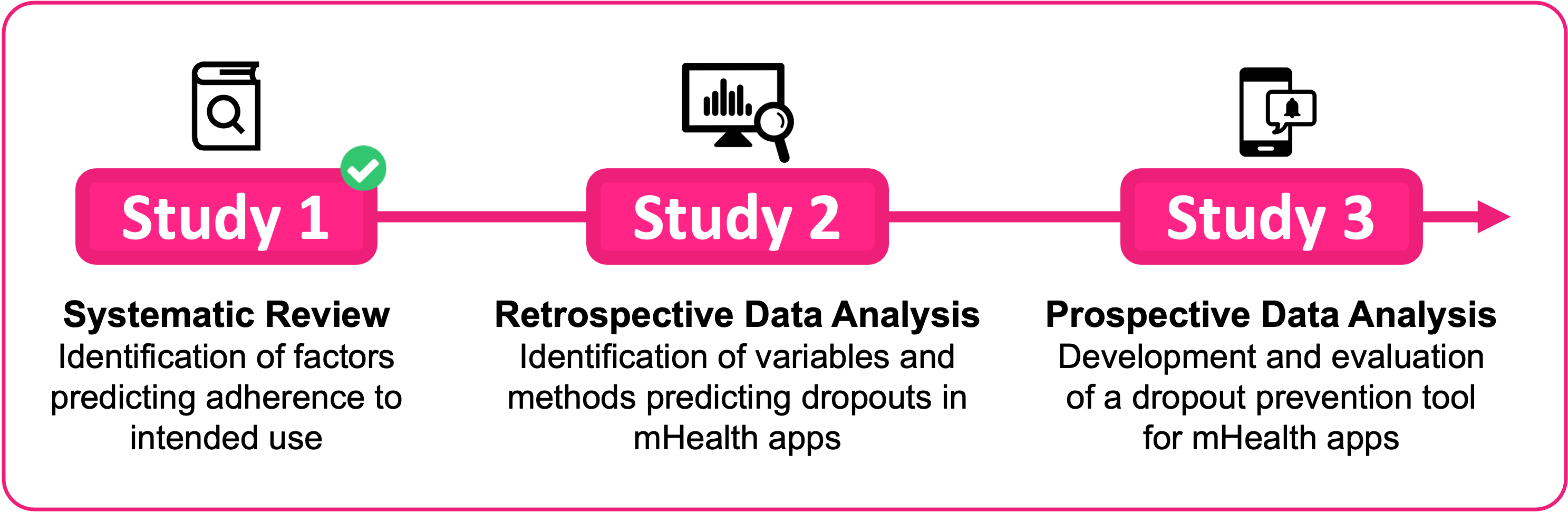
Study 1: Systematic Literature Review
Conducted in cooperation with the Swiss Institute for Addiction and Health Research (ISGF) and funded by the Swiss Federal Office of Public Health, Study 1 aimed to identify intervention- and patient-related factors influencing adherence to the intended use of mHealth apps. We further derived quantified adherence scores for different health domains, which may serve as adherence benchmarks.
A comprehensive systematic literature search (January 2007- December 2020) was conducted in MEDLINE, Embase, Web of Science, Scopus, and ACM Digital Library. Data on intended use, actual use, and factors influencing adherence were extracted. Intervention-related and patient-related factors with a positive or negative influence on app use are presented separately for the health domains NCD-Self-Management, Mental Health, Substance Use, Nutrition, Physical Activity, Weight Loss, Multicomponent Lifestyle Interventions, Mindfulness, and other NCDs. Quantified measures of adherence were derived for each study and compared with qualitative findings.
The following research questions are addressed in Study 1:
- RQ 1.1: Which intervention-related factors influence adherence relative to the intended use of mHealth applications targeting NCDs in adults?
- RQ 1.2: Which patient-related factors influence adherence relative to the intended use of mHealth applications targeting NCDs in adults?
- RQ 1.3: How do adherence rates of mHealth apps for NCDs compare across different health domains?
The results of Study 1 can be found in the corresponding publication which is accessible via the following link: https://jmir.org/2022/5/e35371 [31]
Study 2: Retrospective Data Analysis
In study 2, we strive to identify variables (e.g., login rates, session length, or interaction frequency with specific features) and methods (e.g., logistic regression, decision trees, or random forest models) that effectively predict dropouts in mHealth apps. We also aim to identify intervention components affecting intervention adherence during the process, thus validating and potentially adding to the findings from Study 1. Furthermore, we are going to visualize cohort retention rates and compare them across different mHealth apps, which may grant further insights into common points of dropouts. For this purpose, we collaborate with the following industry project partners:
Manoa – Pathmate Technologies AG (Website)
The digital coach Manoa supports self-managing high blood pressure, type 2 diabetes, and sleep problems in everyday life and motivates users to reduce influenceable risk factors. The app was developed with medical experts and supports the correct documentation of relevant data (e.g., blood pressure, blood glucose, sleep), calculates average values, and provides feedback based on the current state of scientific knowledge and medical guidelines. Manoa is the name of the Pathmate Coach, which is registered as a medical device class I.
Ready4life – Swiss Institute for Addiction and Health Research – ISGF (Website)
The lifestyle intervention ready4life promotes coping with stress, strengthening social skills, and resisting addictive substances. Targeting young people from 15 to 25 years, the app is aimed at learners in vocational schools, polytechnic schools, and training companies in Germany, Liechtenstein, Switzerland, and Austria. Within the app, users can choose a coach (avatar) to guide them through the program.
MySwissFoodPyramid – the Federal Food Safety and Veterinary Office – BLV (Website)
The nutrition app “MySwissFoodPyramid” aims at increasing food literacy in the Swiss population by an interactive food diary and personalized feedback through the MobileCoach-based chat interface and the digital coaches Lukas or Anna. The app is based on Swiss dietary recommendations and aims at people aged 16 and older. The Federal Food Safety and Veterinary Office (BLV) developed the app in collaboration with Pathmate Technologies.
lvlUP – Singapore ETH-Centre (Website)
The holistic lifestyle interbention “lvlUP” aims at supporting adolescents in Singapore with physical exercise, stress management, and healthy eating habits. LvL UP includes several tools, including chatbot coaching, a gameful slow-paced breathing game, and journaling.
WayBetter – WayBetter, Inc. (Website)
WayBetter is a weight management intervention utilizing gamification to motivate users to build new healthy eating and exercise habits, helping users stay accountable to sticking to new habits, and providing users with a supportive community. So far, 1.3 million players have already lost 14.7 million pounds using WayBetter.
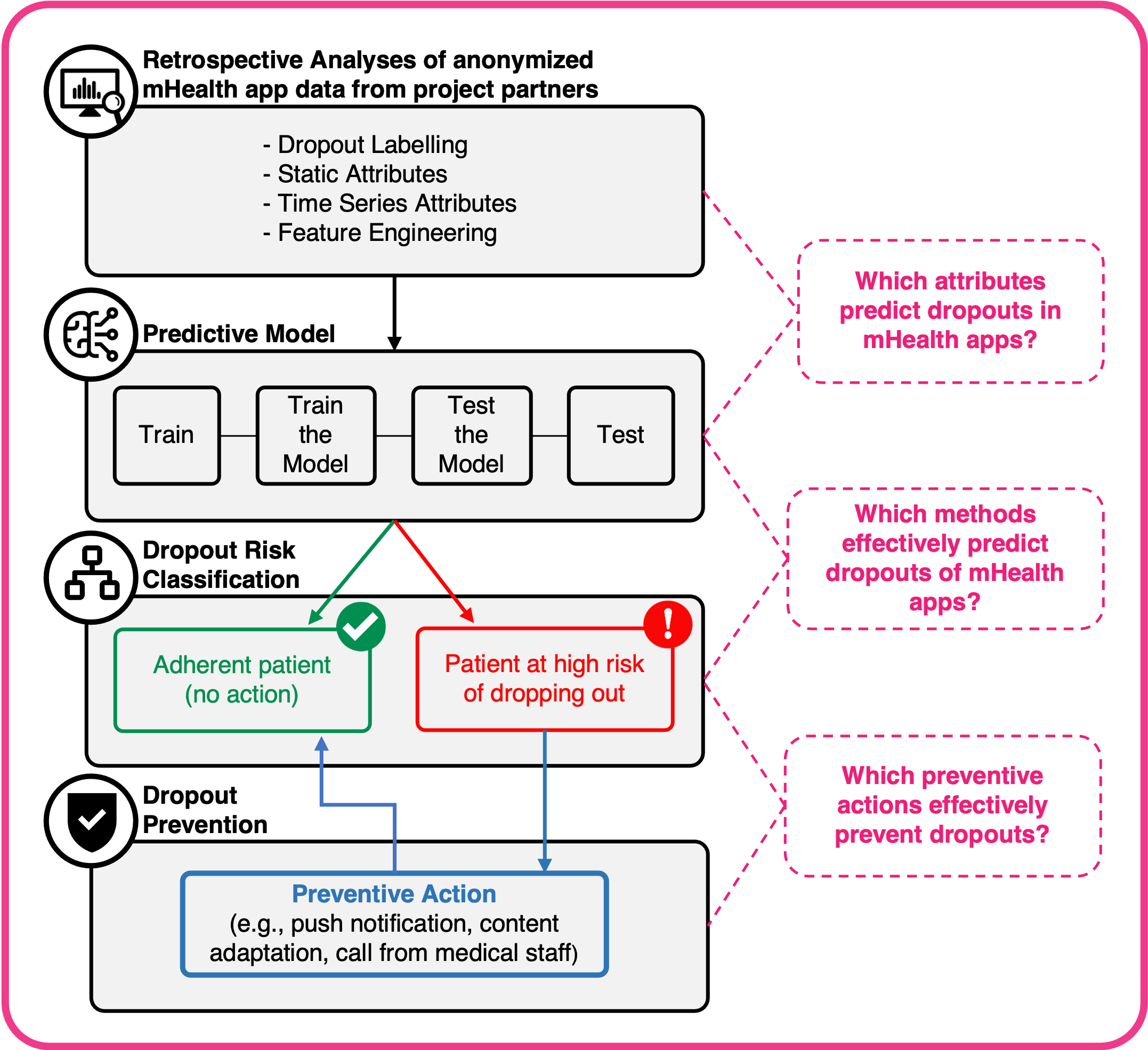
To find effective variables and methods to predict dropouts within these interventions, we will explore a variety of machine learning techniques that have been successfully applied for customer churn prediction in healthcare [14, 17-19], but also other areas such as telecommunications [22-24] or gaming [25-29].
In summary, Study 2 addresses the following research questions:
- RQ 2.1: Which variables predict dropouts in mHealth apps? (e.g., login rates, session length, or interaction frequency with specific features)
- RQ 2.2: Which methods effectively predict dropouts of patients in mHealth apps? (e.g., logistic regression, decision trees, or random forest models
Study 3: Prospective Analysis and Outcome Validation
Applying findings from Studies 1 & 2, we develop and evaluate a prototype of an early warning system that predicts and prevents intervention dropouts. As part of Study 3, we plan to assess the efficacy of this tool with one of our project partners.
In a first step, the tool is supposed to predict dropouts processing adequate real-time socio-demographic, medical, and usage data derived from Studies 1 & 2 applying methods derived from Study 2. In a second step, once a dropout is predicted for a specific user, the tool triggers a preventive action based on findings from Studies 1 & 2. The tool’s efficacy will be evaluated by comparing dropout predictions with actual dropout data and comparing dropout rates of the intervention group (receiving preventive action) with dropout rates of a control group.
The outcome validation of Study 3 aims to answer the following research question:
- RQ 3: Are selected actions effective in preventing dropouts?
Publications
Mair JL, Salamanca-Sanabria A, Frese B, Abend S, Jakob R, Kowatsch T, Haug S. 2023. Effective Behavior Change Techniques in Digital Health Interventions for the Prevention or Management of Noncommunicable Diseases: An Umbrella Review. Annals of Behavioral Medicine. DOI: 10.1093/abm/kaad041
Jakob R, Harperink S, Rudolf A, Fleisch E, Haug S, Mair J, Salamanca-Sanabria A, Kowatsch T. 2022. Factors Influencing Adherence to mHealth Apps for Prevention or Management of Noncommunicable Diseases: Systematic Review. J Med Internet Res 2022;24(5):e35371. DOI: 10.2196/35371
Paz Castro R, Haug S, Debelak R, Jakob R, Kowatsch T, Schaub M. Engagement With a Mobile Phone–Based Life Skills Intervention for Adolescents and Its Association With Participant Characteristics and Outcomes: Tree-Based Analysis. J Med Internet Res 2022;24(1):e28638. DOI:10.2196/28638
Federal Office of Public Health of the Swiss Confederation (BAG). Fact sheet: Success factors of mHealth applications. 2022. URL: https://www.prevention.ch/article/erfolgsfaktoren-von-mhealth-applikationen
Haug S, Augsburger M, Jakob R, Kowatsch T. Literature study on behavioral changes through mHealth applications. 2021. Federal Office of Public Health of the Swiss Confederation (BAG). DOI: 10.3929/ethz-b-000549326.
Related Work
- WHO. Noncommunicable diseases. 2021.
- Suisse e. eHealth Suisse. 2020.
- Olff M. Mobile mental health: a challenging research agenda. Eur J Psychotraumatol. 2015;6:27882. PMID: 25994025. doi: 10.3402/ejpt.v6.27882.
- Wang Y, Xue H, Huang Y, Huang L, Zhang D. A Systematic Review of Application and Effectiveness of mHealth Interventions for Obesity and Diabetes Treatment and Self-Management. Adv Nutr. 2017 May;8(3):449-62. PMID: 28507010. doi: 10.3945/an.116.014100.
- Shaw J, Agarwal P, Desveaux L, Palma DC, Stamenova V, Jamieson T, et al. Beyond “implementation”: digital health innovation and service design. NPJ Digit Med. 2018;1:48. PMID: 31304327. doi: 10.1038/s41746-018-0059-8.
- Aitken M, Clancy, B., & Nass, D. The Growing Value of Digital Health – Evidence and Impact on Human Health and the Healthcare System. 2017.
- Hesser H. Estimating causal effects of internet interventions in the context of nonadherence. Internet Interv. 2020 Sep;21:100346. PMID: 32983907. doi: 10.1016/j.invent.2020.100346.
- Eysenbach G. The law of attrition. J Med Internet Res. 2005 Mar 31;7(1):e11. PMID: 15829473. doi: 10.2196/jmir.7.1.e11.
- Meyerowitz-Katz G, Ravi S, Arnolda L, Feng X, Maberly G, Astell-Burt T. Rates of Attrition and Dropout in App-Based Interventions for Chronic Disease: Systematic Review and Meta-Analysis. J Med Internet Res. 2020 Sep 29;22(9):e20283. PMID: 32990635. doi: 10.2196/20283.
- Linardon J, Fuller-Tyszkiewicz M. Attrition and adherence in smartphone-delivered interventions for mental health problems: A systematic and meta-analytic review. J Consult Clin Psychol. 2020 Jan;88(1):1-13. PMID: 31697093. doi: 10.1037/ccp0000459.
- Baumel A, Muench F, Edan S, Kane JM. Objective User Engagement With Mental Health Apps: Systematic Search and Panel-Based Usage Analysis. J Med Internet Res. 2019 Sep 25;21(9):e14567. PMID: 31573916. doi: 10.2196/14567.
- Morrissey EC, Corbett TK, Walsh JC, Molloy GJ. Behavior Change Techniques in Apps for Medication Adherence: A Content Analysis. Am J Prev Med. 2016 May;50(5):e143-e6. PMID: 26597504. doi: 10.1016/j.amepre.2015.09.034.
- Sieverink F, Kelders SM, van Gemert-Pijnen JE. Clarifying the Concept of Adherence to eHealth Technology: Systematic Review on When Usage Becomes Adherence. J Med Internet Res. 2017 Dec 6;19(12):e402. PMID: 29212630. doi: 10.2196/jmir.8578.
- Pedersen DH, Mansourvar M, Sortsø C, Schmidt T. Predicting Dropouts From an Electronic Health Platform for Lifestyle Interventions: Analysis of Methods and Predictors. J Med Internet Res. 2019;21(9):e13617. PMID: 31486409. doi: 10.2196/13617.
- Trinh H, Shamekhi A, Kimani E, Bickmore TW. Predicting User Engagement in Longitudinal Interventions with Virtual Agents. Proceedings of the 18th International Conference on Intelligent Virtual Agents; Sydney, NSW, Australia: Association for Computing Machinery; 2018. p. 9–16.
- Baumel A, Yom-Tov E. Predicting user adherence to behavioral eHealth interventions in the real world: examining which aspects of intervention design matter most. Transl Behav Med. 2018 Sep 8;8(5):793-8. PMID: 29471424. doi: 10.1093/tbm/ibx037.
- Bremer V, Chow PI, Funk B, Thorndike FP, Ritterband LM. Developing a Process for the Analysis of User Journeys and the Prediction of Dropout in Digital Health Interventions: Machine Learning Approach. J Med Internet Res. 2020 Oct 28;22(10):e17738. PMID: 33112241. doi: 10.2196/17738.
- Kwon H, Kim HH, An J, Lee JH, Park YR. Lifelog Data-Based Prediction Model of Digital Health Care App Customer Churn: Retrospective Observational Study. J Med Internet Res. 2021 Jan 6;23(1):e22184. PMID: 33404511. doi: 10.2196/22184.
- SARINE BABIKIAN VS, MARK A. CLEMENTS. 862-P: A Machine Learning Model Predicts Engagement with a Mobile Health (mHealth)-Based Remote Patient Monitoring (RPM) Program among Persons with Diabetes (PWDs). Diabetes Jun 2020, 69 (Supplement 1) 862-P. 2020. doi: 10.2337/db20-862-P.
- Kramer JN, Kunzler F, Mishra V, Presset B, Kotz D, Smith S, et al. Investigating Intervention Components and Exploring States of Receptivity for a Smartphone App to Promote Physical Activity: Protocol of a Microrandomized Trial. JMIR Res Protoc. 2019 Jan 31;8(1):e11540. PMID: 30702430. doi: 10.2196/11540.
- Künzler F, Mishra V, Kramer J-N, Kotz D, Fleisch E, Kowatsch T. Exploring the State-of-Receptivity for mHealth Interventions. Proc ACM Interact Mob Wearable Ubiquitous Technol. 2019;3(4):Article 140. doi: 10.1145/3369805.
- Raja B, Jeyakumar P. An Effective Classifier for Predicting Churn in Telecommunication. Journal of Advanced Research in Dynamical and Control Systems. 2019 06/07;11:221-9.
- Vafeiadis T, Diamantaras KI, Sarigiannidis G, Chatzisavvas KC. A comparison of machine learning techniques for customer churn prediction. Simulation Modelling Practice and Theory. 2015 2015/06/01/;55:1-9. doi: https://doi.org/10.1016/j.simpat.2015.03.003.
- Ahmad AK, Jafar A, Aljoumaa K. Customer churn prediction in telecom using machine learning in big data platform. Journal of Big Data. 2019 2019/03/20;6(1):28. doi: 10.1186/s40537-019-0191-6.
- Kawale J, Pal A, Srivastava J, editors. Churn Prediction in MMORPGs: A Social Influence Based Approach. 2009 International Conference on Computational Science and Engineering; 2009 29-31 Aug. 2009.
- Hadiji F, Sifa R, Drachen A, Thurau C, Kersting K, Bauckhage C, editors. Predicting player churn in the wild. 2014 IEEE Conference on Computational Intelligence and Games; 2014 26-29 Aug. 2014.
- Á P, Saas A, Guitart A, Magne C, editors. Churn Prediction in Mobile Social Games: Towards a Complete Assessment Using Survival Ensembles. 2016 IEEE International Conference on Data Science and Advanced Analytics (DSAA); 2016 17-19 Oct. 2016.
- Bertens P, Guitart A, Á P, editors. Games and big data: A scalable multi-dimensional churn prediction model. 2017 IEEE Conference on Computational Intelligence and Games (CIG); 2017 22-25 Aug. 2017.
- Runge J, Gao P, Garcin F, Faltings B, editors. Churn prediction for high-value players in casual social games. 2014 IEEE Conference on Computational Intelligence and Games; 2014 26-29 Aug. 2014.
- Mishra H, Enami S, Nielsen RJ, Stewart LA, Hoffmann MR, Goddard WA, 3rd, et al. Bronsted basicity of the air-water interface. Proc Natl Acad Sci U S A. 2012 Nov 13;109(46):18679-83. PMID: 23112167. doi: 10.1073/pnas.1209307109.
- Jakob R, Harperink S, Rudolf AM, Fleisch E, Haug S, Mair JL, Salamanca-Sanabria A, Kowatsch T. Factors Influencing Adherence to mHealth Apps for Prevention or Management of Noncommunicable Diseases: Systematic Review. J Med Internet Res 2022;24(5):e35371. doi: 10.2196/35371 . PMID: 35612886
Research Team
M.Sc. Robert Jakob
Prof. Dr. Tobias Kowatsch
Prof. Dr. Elgar Fleisch
Dr. Alicia Salamanca
Dr. Jacqueline Mair
PD Dr. rer. med. habil. Dr. phil. Dipl.-Psych Severin Haug
Dr. med. Aaron Maria Rudolf
M.Sc. Samira Harperink
M.Sc. Justas Narauskas
M.Sc. Jannis Laufer
M.Sc. Yili Toby Yang
M.Sc. Nils Lepper
M.Sc. Flurin Müller
Runtime
Sep 2020 – Aug 2024