Digital Health Project Course, Spring Semester 2021, University of St.Gallen
The promise of more personalized, patient‐centered and outcomes‐based healthcare is real, worthy, and within reach (Harvard Business Review, October 2019), NHS teams up with Amazon to bring Alexa to patients (The Guardian, July 2019), Apple Heart Study demonstrates ability of wearable technology to detect atrial fibrillation (Stanford Medicine News, March 2019), Industries like healthcare are quietly adopting chatbots to free up busy professionalsʹ time and offer guided, personalized experiences to consumers (CB Insights, October 2019), Digital health companies raised a total of $4.2B across 180 deals through the first half of 2019. If this pace holds steady, the sector is on track for an $8.4B year in 2019 ‐ and may even top 2018ʹs record‐breaking annual funding total. (Sean Day, Rocket Health, 2019 Midyear Digital Health Market Update)
What are the implications and rationale behind the recent developments in the field of digital health?
Digital Health is the use of information and communication technology for the prevention and treatment of diseases in the everyday life of individuals. It is thus linked to topics such as digital health interventions, digital biomarker, digital coaches and healthcare chatbots, telemedicine, mobile and wearable computing, self‐tracking, personalized medicine, connected health, smart homes or smart cars.
In the 20th century, healthcare systems specialized in acute care. In the 21st century, we now face the challenge of dealing with the specific characteristics of chronic conditions. These are now responsible for around 70% of all deaths worldwide and 85% of all deaths in Europe and are associated with an estimated economic loss of $7 trillion between 2011 and 2025. Chronic diseases are characterized in particular by the fact that they require an intervention paradigm that focuses on prevention and lifestyle change. Lifestyle (e.g., diet, physical activity, tobacco, or alcohol consumption) can reduce the risk of suffering from a chronic condition or, if already present, can reduce its burden. A corresponding change in lifestyle is, however, only implemented by a fraction of those affected, partly because of missing or inadequate interventions or health literacy, partly due to socio‐cultural influences. Individual personal coaching of these individuals is neither scalable nor financially sustainable.
Against this background, the question arises on how to develop evidence‐based digital health interventions (DHIs) that allow medical doctors and other caregivers to scale and tailor long‐term treatments to individuals in need at sustainable costs. At the intersection of health economics, information systems research, computer science, and behavioral medicine, this lecture has the objective to help students and upcoming healthcare executives interested in the multi‐disciplinary field of digital health to better understand the need, design, implementation, and assessment of DHIs.
After the course, students will be able to…
- understand the importance of DHIs for the management of chronic conditions
- discuss the opportunities and challenges related to DHIs
- better understand the design, implementation and evaluation of smartphone‐based and chatbot‐delivered DHIs
To reach the learning objectives, students will work on the following topics:
1. Motivation for Digital Health
- The rise of chronic diseases in developed countries
- Lifestyle as medicine and prevention of chronic diseases
2. Design of a Digital Health Intervention (DHI)
- Overview of design frameworks for health interventions
- Development of a conceptual model for a DHI
- Implementation of a smartphone‐based and chatbot‐delivered DHI
3. Evaluation of DHIs
- Overview of evaluation methods and evaluation criteria for DHIs
- Evaluation of a smartphone‐based and chatbot‐delivered DHI
Course Structure
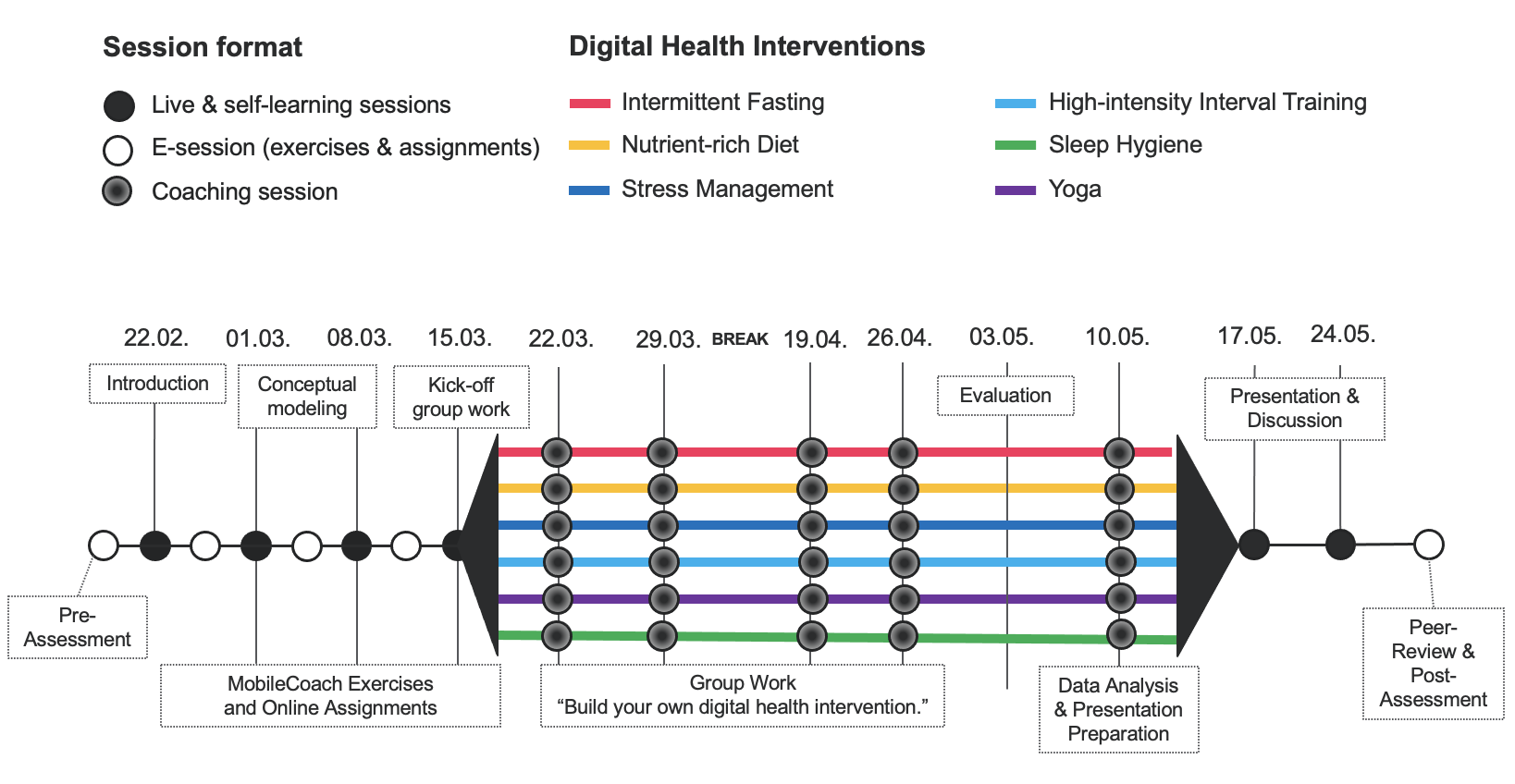
The lecture is structured in two parts and follows the concept of a hybrid therapy consisting of online sessions via Zoom and complementary self-learning sessions. In the first part, students will learn about the topics of the three learning modules in weekly online sessions. Complementary learning material (e.g., video clips), multiple‐choice questions, and exercises are provided online via Canvas.
In the second part, students work in teams and will use their knowledge from the first part to develop a smartphone-based and chatbot-delivered health intervention with MobileCoach (www.mobile-coach.eu), an open‐source software platform for digital interventions and ecological momentary assessments. Each team will then present and discuss their resulting digital health intervention and evaluation results with their fellow students who will provide peer-reviews. Additional online coaching sessions are offered to support the teams with the design and evaluation of their digital health intervention, and with the preparation of their presentations.
Course Literature
- Collins, L. M. (2018) Optimization of Behavioral, Biobehavioral, and Biomedical Interventions: The Multiphase Optimization Strategy (MOST) New York: Springer.
- Corneta, V. P., and R. J. Holden (2018) Systematic Review of Smartphone‐Based Passive Sensing for Health and Wellbeing Journal of Biomedical Informatics (77:January), 120‐132.
- Coravos, A., S. Khozin and K. D. Mandl (2019) Developing and Adopting Safe and Effective Digital Biomarkers to Improve Patient Outcomes Nature Digital Medicine 2 Paper 14.
- Katz, D. L., E. P. Frates, J. P. Bonnet, S. K. Gupta, E. Vartiainen and R. H. Carmona (2018) Lifestyle as Medicine: The Case for a True Health Initiative American Journal of Health Promotion 32 (6), 1452‐1458.
- Kowatsch, T., L. Otto, S. Harperink, A. Cotti and H. Schlieter (2019) A Design and Evaluation Framework for Digital Health Interventions it ‐ Information Technology 61(5‐6), 253‐263.
- Kvedar, J. C., A. L. Fogel, E. Elenko and D. Zohar (2016) Digital medicineʹs march on chronic disease Nature Biotechnology 34 (3), 239‐246.
- Michie, S., L. Yardley, R. West, K. Patrick and F. Greaves (2017) Developing an Evaluating Digital Interventions to Promote Behaviour Change in Health and Health Care: Recommendations Resulting From an International Workshop Journal of Medical Internet Research 19(6):e232.
- Nahum‐Shani, I., S. N. Smith, B. J. Spring, L. M. Collins, K. Witkiewitz, A. Tewari and S. A. Murphy (2018) Just‐in‐Time Adaptive Interventions (JITAIs) in Mobile Health: Key Components and Design Principles for Ongoing Health Behavior Support Annals of Behavioral Medicine 52 (6), 446‐462.
Mandatory material
The mandatory material will be provided via the online learning platform.
Course Prerequisites
Students should be interested in the multi‐disciplinary field of Digital Health at the intersection of health economics, information systems research, computer science, and behavioral medicine. Attendance of the Digital Health course (7,800) is advantageous but not required.
Please note that you need to set up a mobile application development environment and a smartphone emulator (i.e., React Native in combination with either Android Studio for Windows, Mac, or Linux or XCode for Mac). You will get detailed instructions for the installation and usage of that software. Programming skills may be helpful but are not a requirement in this course.
Moreover, your personal computer must meet the following requirements: (a) Windows 7/8/10 (64‐bit), (b) MacOS 10.14.4 or higher, or (c) Linux GNOME or KDE desktop 64‐bit distribution capable of running 32-bit applications GNU C Library (glibc) 2.19 or later. For each setup, 12 GB of available disk space, a minimum of 4 GB RAM (8 GB RAM recommended), and a 13” display (15” or larger recommended) are required.
Finally, a smartphone with either iOS 12 (or higher) or Android Version 8 (or higher) is required to test the digital health interventions of the course participants.
Additional Course Information
If you have any further questions regarding the Digital Health Project course, please contact David Cleres or Robert Jakob.
Summary
Joint Medical Master, Digital Health Project, University of St.Gallen, Spring Semester 2021, 11,803,1.00, 2 ECTS credits, Online via CANVAS, Mondays, 4:15 p.m. – 6:00 p.m., video clips, HSG Link.